How do you manage urinary incontinence? Urinary incontinence definition
Urinary incontinence is a prevalent condition that significantly affects your physical, psychological, and social well-being, as well as the well-being of your family and caregivers. Estimating its prevalence is challenging due to variations in its definition and the underreporting of continence issues. For men, the prevalence remains largely unknown, with figures ranging from 5.3% to 45.8% of the population.
Currently, there are around 3.4 million men in the USA experiencing this condition. The prevalence of urinary incontinence increases with age and is frequently observed in adults residing in institutions and care homes. However, it is important not to simply accept this situation. Instead, seek assistance as there might be a treatable underlying cause and numerous options available to enhance symptoms, effectively manage the issue, and decrease the likelihood of feeling embarrassed.
Urinary incontinence refers to the involuntary release of urine without control. Several types of urinary incontinence exist:
1. Functional incontinence occurs when an individual is unable to reach the toilet in time due to factors like limited mobility or unfamiliar surroundings.
2. Stress incontinence arises when activities such as bending, lifting, jumping, or coughing exert pressure on the bladder, leading to leaks.
3. Urge incontinence involves experiencing a sudden and urgent need to urinate that cannot be delayed, caused by the bladder contracting inappropriately. This results in an overwhelming and intense urge to urinate, making it difficult to reach the bathroom in time.
4. Mixed urinary incontinence refers to the involuntary release of urine that occurs both during moments of urgency and physical exertion, such as coughing, sneezing, or making an effort.
5. Overactive bladder syndrome (OAB) manifests as a frequent and urgent need to urinate, often including nighttime urination (nocturia). OAB can be categorized as OAB wet or OAB dry. OAB wet denotes the actual release of urine after experiencing the urge, while OAB dry indicates the sensation of urgency without any subsequent release (a form of mixed signals from the bladder).
6. Overflow incontinence occurs when the bladder is unable to fully empty, resulting in unexpected urine leakage. In men, this is frequently caused by prostatic disease, while nerve control issues associated with stroke or Parkinson’s disease can also lead to this condition. Overflow incontinence can give rise to complications involving the kidneys.
URINARY INCONTINENCE IN MEN – RISK FACTORS
Men are at risk of experiencing various factors that can lead to urinary problems. These factors encompass lower urinary tract symptoms, infections, functional and cognitive impairment, neurological disorders such as stroke, dementia, Parkinson’s disease, or nerve damage resulting from injury or surgery, as well as prostatectomy. Additionally, obstruction caused by an enlarged prostate gland or pelvic tumours can also contribute to incontinence.
INVESTIGATIONS
A comprehensive evaluation by a doctor, such as a urologist or physician, is necessary to identify potential causes and the specific type of incontinence. Several tests, including digital rectal examination to assess the prostate, nerve conduction studies, assessment of physical independence, mobility and function, and maintaining a bladder diary, are conducted to diagnose incontinence. The bladder diary involves recording the amount of fluids consumed, frequency of urination, and any incidents of leakage or accidents, along with associated triggers such as heavy lifting, laughter, or driving. Additional tests may include dipstick tests to detect infection, blood, or glucose in the urine, kidney function tests, and pelvic ultrasound to identify any abnormalities.
MANAGEMENT
1. Temporary containment products such as pads, diapers, or collecting devices can assist in achieving ‘social’ continence, enabling individuals to conceal any accidents while at work or socializing. Some men may initially hesitate to use pads or disposable undergarments. However, these products not only prevent embarrassing leaks but also safeguard the skin from irritation and eliminate odour. Moreover, they can help rebuild confidence and allow for a social life beyond the confines of one’s home and bathroom. You might be surprised by the wide range of product options available. Unlike the bulkier ‘adult nappies’ that may come to mind, modern incontinence pads and undergarments are designed to provide comfort and discretion.
After assessing and excluding alternative management methods, it is advisable to only consider using drip collectors – disposable padded sheaths designed to encircle the penis – for minor leaks or dribbles. However, we do not discourage their use as they provide a sense of security in public, allowing for a more liberated and unashamed lifestyle, rather than experiencing isolation.
2. Medication can be beneficial in managing the condition. Certain medications work by inducing muscle relaxation to prevent involuntary bladder contractions. Others function by inhibiting the nerve signals that cause the bladder to contract at inappropriate intervals. Medications prescribed for reducing an enlarged prostate can also alleviate other urinary issues. However, it is important to note that diuretic medications, commonly known as ‘water pills’, may potentially trigger or exacerbate incontinence.
3. Consider either intermittent self-catheterization or using in-dwelling catheters. External catheters function similarly to condoms and collect urine. They are connected to drainage bags, which can be suspended beside your bed while you sleep or strapped to your body discreetly under your clothing during the day. If you experience overflow incontinence, it may be beneficial to explore intermittent catheterization, wherein a tube is inserted through your urethra into your bladder at specific intervals to ensure regular emptying and minimize leakage. Consult your doctor for further guidance.
4. Surgical interventions can address incontinence, such as the male sling procedure for stress incontinence. This involves wrapping material around the urethra to exert pressure and prevent leakage during activities like coughing, sneezing, or exertion. Another option is the implantation of an artificial sphincter, which utilizes a cuff to close off the urethra. By squeezing a pump, the cuff is opened, allowing urine to be released at will. Additionally, a device resembling a pacemaker can be employed to stimulate nerves that relax the bladder and pelvic floor muscles.
5. Pelvic floor muscle retraining involves exercise therapy with a physical therapist to boost the strength of the pelvic muscles responsible for bladder control. Kegel exercises, which can be easily incorporated into a daily routine, aid in improving the ability to hold urine.
6. Electrical stimulation and biofeedback are treatment methods used in conjunction with physical therapy. During this procedure, electrodes are positioned on the muscles, and a monitor displays immediate feedback on the contractions of the muscles surrounding the bladder. Through practice, you can acquire the skill of relaxing your body, relieving muscle tension, enhancing control, and correctly sequencing muscle contractions. This progressive approach will ultimately lead to an improvement in your symptoms.
7. Bladder training involves a behavioural approach. Initiate the process by emptying your bladder every 30 minutes, regardless of whether you feel the need to urinate or not. Gradually increase the time intervals between bathroom visits over a period of days or weeks. Eventually, you may be able to extend the gaps between breaks to 3 to 4 hours, which can help reduce the frequency of urges. Keep track of your fluid intake.
8. Some men find success by spacing out their consumption of fluids throughout the day and reducing their intake a few hours before bedtime. If this strategy proves effective for you, continue following it. However, be cautious not to restrict your fluid intake excessively, as it may lead to dehydration. Insufficient hydration can result in complications such as bladder infections, which can further exacerbate urinary incontinence.
9. Consider your beverage choices carefully. Consuming caffeinated drinks may aggravate your bladder as they act as diuretics, exacerbating symptoms. Carbonated drinks, including soda, can have a similar effect. Additionally, alcohol acts as a diuretic, increasing urine production. Try reducing your intake of tea, coffee, soda, and alcohol to see if it positively impacts your condition.
10. Monitor your food intake and be mindful of what you consume. Certain individuals have observed that the consumption of spicy or acidic foods can exacerbate urinary incontinence linked to OAB. Additionally, some have reported that avoiding chocolate and artificial sweeteners is helpful. It is important to note that specific triggers may vary between individuals, and some people may not notice any impact from their diet. To identify potential triggers, maintain a food diary to track your intake. Gradually reduce the consumption of one food item at a time for a week to determine if there are any changes in your symptoms.
11. Minimize stress. Dealing with incontinence can be a source of stress. Employing relaxation techniques such as deep breathing exercises, meditation, gentle exercise, or receiving a massage can aid in managing symptoms. Be prepared. Unexpected instances of urinary incontinence may occur. Take note of the restroom locations upon entering establishments like restaurants or stores to ensure swift access. If planning a car journey, carefully plan the route and determine appropriate restroom stops. Opt for clothing that can be easily removed in urgent situations. Additionally, it is advisable to keep spare pads and a plastic urinal in the car for emergencies, such as getting caught in a traffic jam.
12. Seek assistance. Constant worry about incontinence can lead to exhaustion and detrimental effects on your social life, possibly causing a reluctance to venture outside. If this has become your reality, take action to alter it. Explore options such as joining a support group, consulting a therapist, or revisiting your doctor for alternative solutions. Keep in mind that incontinence is typically treatable.
Urinary incontinence – PELVIC FLOOR EXERCISES
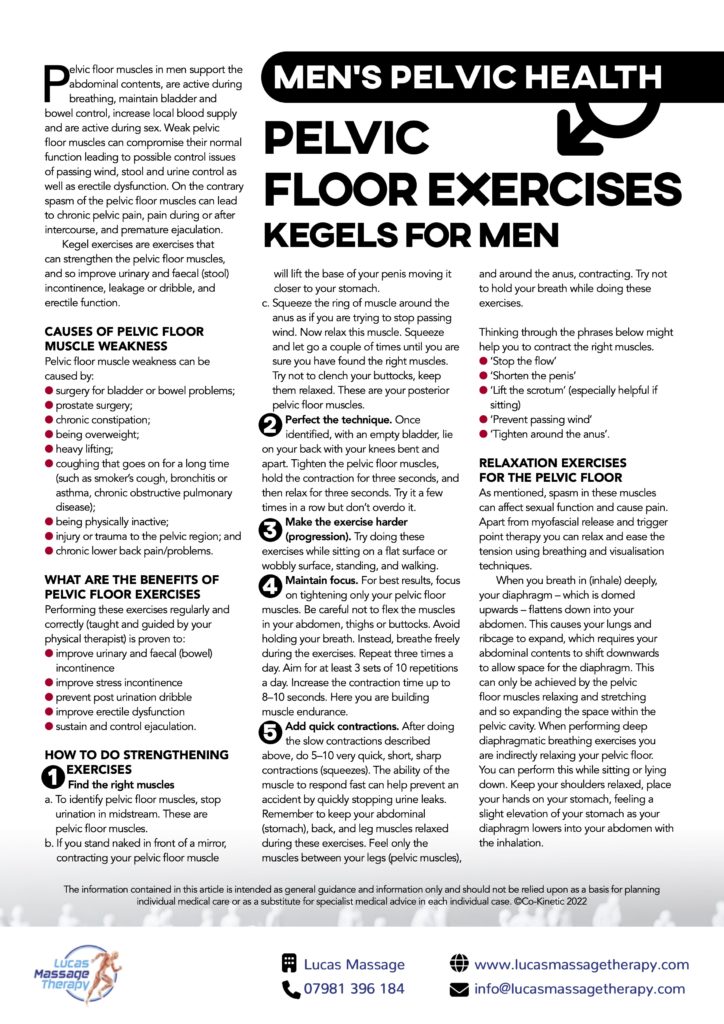
We’re talking bladder control, bowel movements and yep, the reproductive organs as well. All these crucial functions are controlled by muscles in the pelvis.
Dysfunction in any of these areas is something you need to see a doctor about asap. In some cases, symptoms can be a sign of a more serious health problem such as prostate cancer.
What Are ‘Pelvic Health’ Problems?
Issues in the pelvic region vary greatly, from pain to leaky bladders or bowels to sexual dysfunction problems like premature ejaculation. They’re also more common than you might think, and most are easily managed or treated once medical help has been requested.
FREE – Men’s Pelvic Health Resource Pack
Download our Lucas Massage Therapy free information pack and find out everything you need to know about men’s pelvic health.
What You’ll Learn:
- The different signs and symptoms to look out for in the pelvic region
- When symptoms might indicate prostate cancer
- How pelvic health conditions are treated
- The dangers of ‘staying silent’
- How a few simple exercises can make a big difference to your pelvic health

