Prostate cancer
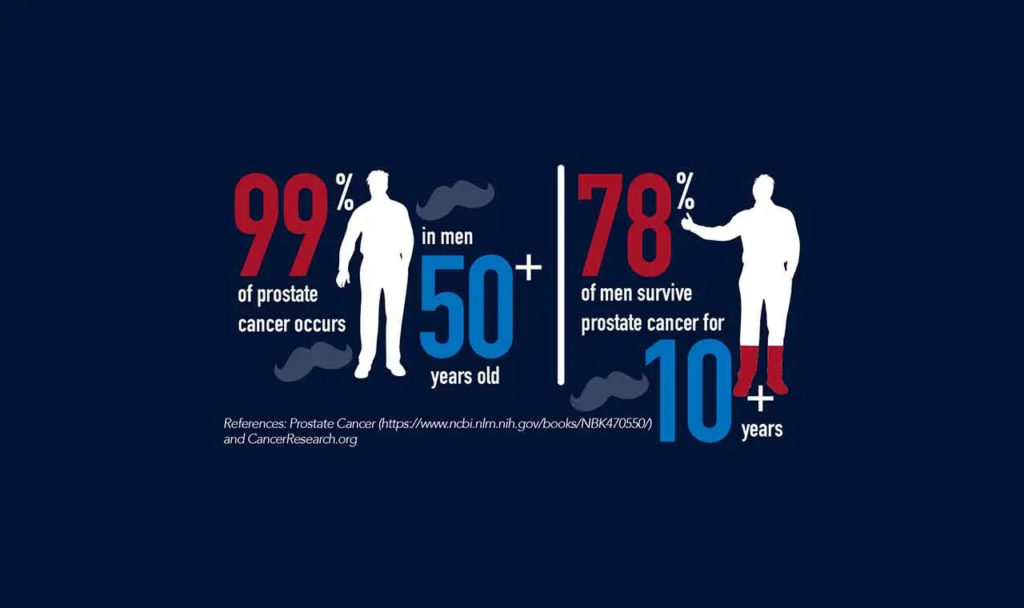
Prostate cancer is the second most common cause of cancer-related death in men and the most prevalent cancer type in men following skin cancer. It originates in the prostate gland, a component of the male reproductive system responsible for producing seminal fluid. This cancer grows slowly and affects approximately one-third of men by the age of 50. It can spread to other organs, primarily the bones in the pelvic region such as the hip or lower back.
Bone cancer can cause pain and mobility issues. Few prostate cancer patients die from the disease. On one hand, it can be slow-growing in some men and not cause any health problems or symptoms. Without regular check-ups, it might go unnoticed in these individuals. On the other hand, many men choose to stay silent about pelvic issues and avoid pelvic exams during routine check-ups due to shame, embarrassment, or fear. The prevalence of prostate cancer appears to have increased, possibly due to unhealthy lifestyle choices or more men undergoing regular screening. Globally, approximately 1 in 7 men will receive a prostate cancer diagnosis. However, advancements in treatment have allowed more men to live longer with the disease.
Prostate cancer signs – Prostate cancer symptoms
These signs can occur in prostate cancer as well as other prostate-related conditions like benign prostatic hyperplasia (BPH) or prostatitis (chronic pelvic pain syndrome). The symptoms may include: urinary retention or other urinary issues, low back pain, pain or stiffness in the inner thigh or perineal area (between the anus and scrotum), haematuria (blood in the urine), blood in semen, suprapubic pain or discomfort (in the lower abdominal/pubic hair area and base of the penis), pelvic pain that extends towards the genital area and hips, and sexual dysfunction. Early prostate cancer may not show any symptoms.
Prostate cancer is commonly detected through routine screenings in men without symptoms. Early diagnosis is crucial for better outcomes. Metastasized cancer may cause additional symptoms, including sciatica, bone and leg pain, swelling in the groin and leg, tingling or numbness in the pelvis, perineum, and legs, anemia, weight loss or loss of appetite, dark stools, and changes in bladder or bowel function. Screening methods for diagnosis may involve a blood test for PSA, rectal examination to assess prostate gland enlargement, and ultimately, a biopsy of the prostate gland to confirm the presence of cancer cells.
The diagnostic process for prostate cancer involves different tests, including a blood test to measure prostate-specific antigen (PSA) levels and a rectal examination to evaluate prostate gland enlargement. Confirming the presence of prostate cancer requires a biopsy of the prostate gland, particularly for individuals with elevated PSA levels. A tiny sample of the prostate gland is extracted and examined under a microscope to detect cancer cells.
PROSTATE CANCER STAGES
Stage 1
Cancer is not detectable through a digital rectal examination (DRE), but it may be incidentally discovered during unrelated surgery. The cancer has not metastasized to other regions.
Stage 2
Cancer can be detected through a DRE or identified through a biopsy. The cancer has not spread beyond its original location.
Stage 3
Cancer has spread to nearby tissue.
Stage 4
Cancer has spread to lymph nodes or distant body parts.
The exact cause of prostate cancer remains unknown; however, there exist various established risk factors that have been linked to an increased likelihood of developing this form of cancer. Unmodifiable risk factors include l age (rarely seen before the age of 45);
1. ethnicity (more prevalent in African American men compared to white or Hispanic men);
2. geographical location (higher occurrence in North America, north-western Europe, Australia, and the Caribbean islands, while less common in Asia, Africa, Central, and South America);
3. family history;
4. viruses; and l hormones.
Risk factors that you can attempt to manage and modify consist of dietary choices (a diet rich in animal fat, red meat, and high-fat dairy products may contribute to an elevated risk of developing prostate cancer); obesity; exposure to certain substances in the workplace, like chemicals (such as herbicides, pesticides, and toxic flammable products), cadmium, and other metals; engaging in sexual activity with multiple partners; and having low levels of vitamins and selenium. It is crucial to consider one’s overall health status, not just age when screening for cancers. The mortality (death) rate associated with prostate cancer is influenced by co-existing medical conditions, including chronic respiratory disease, diabetes, and being overweight or obese.
MANAGEMENT
Determining whether treatment is necessary is the initial step in managing prostate cancer. Prostate cancer, particularly low-grade tumors, tends to have a slow growth rate. Patients may opt for active surveillance, which involves regular PSA testing and an additional biopsy 12 to 18 months after diagnosis. It’s worth considering the potential side effects of treatment, such as erectile dysfunction and urinary or fecal incontinence, when discussing the treatment’s objectives (potential cancer cure, increased survival, emotional relief) versus the risks associated with lifestyle changes (treatment side effects, complications, cost, potential lack of long-term survival benefit).
Treatment for prostate cancer may involve external beam radiation therapy targeting the cancer cells, or brachytherapy which entails the insertion of radioactive pellets to eliminate the cancer cells. Another option is radical prostatectomy, a surgical procedure to remove the prostate gland and potentially surrounding tissue. Cryotherapy, typically used when radiation therapy is unsuccessful, is also employed. Radiation therapy generally has significantly fewer side effects (approximately 50% less) compared to radical prostatectomy surgery, while offering similar overall survival rates. Chemotherapy, administered orally or intravenously, is used to kill or shrink the cancer cells.
Hormonal treatment is additionally employed to decrease the absorption of testosterone by malignant cells, thereby impeding their proliferation. An individualized vaccine for each patient may be developed to enhance the immune system’s ability to eliminate prostate cancer cells. This approach is primarily utilized for advanced cases where hormone therapy is ineffective. The curability of metastasized prostate cancer is uncommon. Managing the condition involves employing medications and drugs to further diminish the cancer’s size and extent, as well as alleviate symptoms such as bone pain through analgesic administration.
PHYSICAL THERAPY MANAGEMENT
Typical issues associated with genito-urinary cancer (cancer affecting the genitals, bladder, pelvis, or surrounding areas) include:
– Reduced physical strength
– Incontinence (a prevalent side effect of prostate cancer treatment)
– Impaired genito-urinary function (e.g., erectile dysfunction)
– Pain
– Fatigue
– Peripheral neuropathy (abnormal nerve signals such as tingling and numbness)
– Lymphedema (persistent swelling in the groin and legs)
Physical therapy treatment may include:
1. Strengthening and coordinating the pelvic floor muscles through pelvic floor muscle training can enhance urinary control and prevent leaks. Women who have undergone childbirth, hysterectomy, pelvic surgeries, or reached menopause are often recommended to perform Kegels and other pelvic floor exercises. Men have similar pelvic floor muscles, so they should also engage in similar exercises. Pelvic pain can arise from muscle spasms or tightness in the pelvic floor, which can cause pain in the pelvic region. Learning to relax these muscles may aid in pain reduction.
2. Biofeedback training, which utilizes small electrodes to effectively stimulate the pelvic floor muscles and ensure optimal contraction in the correct sequence, is a widely accepted method for addressing incontinence and aiding in the recovery of erectile dysfunction. It is important not to overlook this approach, particularly for women, as it has a proven track record of success.
3. Trigger point therapy is a technique used to manually release tense and congested areas in the pelvic floor muscles. These areas can cause pain and hinder proper muscle function. Physical therapists have the expertise to address various health concerns. They can provide guidance on developing a physical activity plan that includes targeted aerobic training and strength exercises to manage and prevent cancer-related fatigue. Furthermore, they can assist with weight management and overall health, leading to improved prognosis and mental well-being.
PELVIC FLOOR EXERCISES
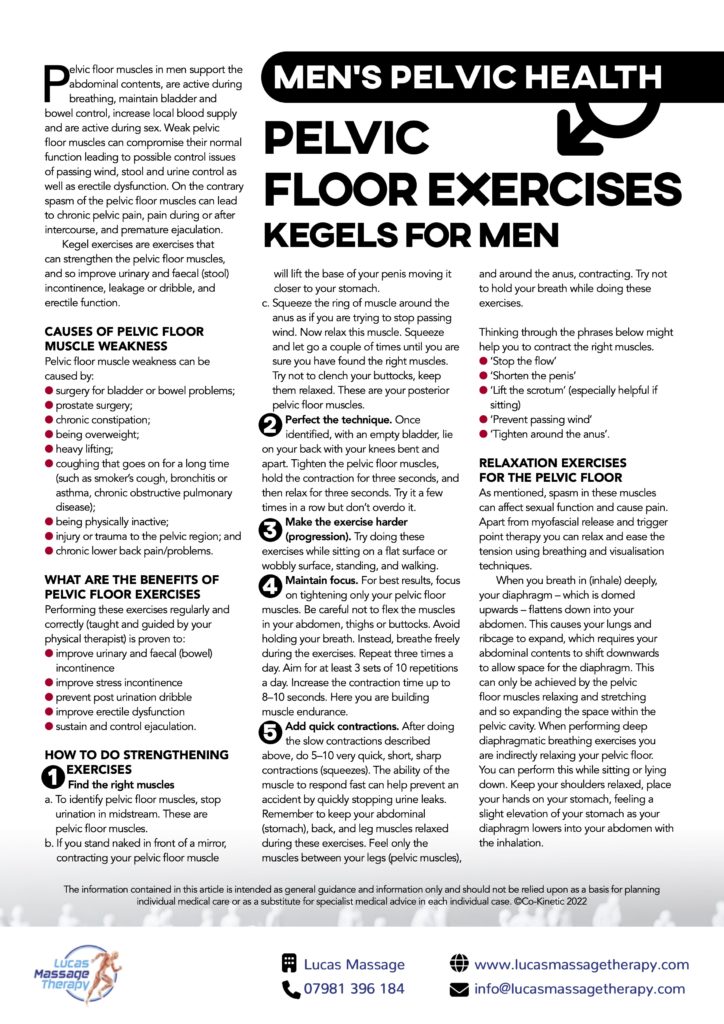
We’re talking bladder control, bowel movements and yep, the reproductive organs as well. All these crucial functions are controlled by muscles in the pelvis.
Dysfunction in any of these areas is something you need to see a doctor about asap. In some cases, symptoms can be a sign of a more serious health problem such as prostate cancer.
What Are ‘Pelvic Health’ Problems?
Issues in the pelvic region vary greatly, from pain to leaky bladders or bowels to sexual dysfunction problems like premature ejaculation. They’re also more common than you might think, and most are easily managed or treated once medical help has been requested.
FREE – Men’s Pelvic Health Resource Pack
Download our Lucas Massage Therapy free information pack and find out everything you need to know about men’s pelvic health.
What You’ll Learn:
- The different signs and symptoms to look out for in the pelvic region
- When symptoms might indicate prostate cancer
- How pelvic health conditions are treated
- The dangers of ‘staying silent’
- How a few simple exercises can make a big difference to your pelvic health

