Chronic Pelvic Pain in Men
Male chronic pelvic pain syndrome (CPPS) is a prevalent urological condition involving the bladder, kidneys, their tracts, and the prostate. It is a form of prostatitis, also known as chronic prostatitis, although this term can be misleading as it suggests prostate involvement and inflammation, which is not always the case. CPPS is a non-bacterial manifestation of the disease characterized primarily by pain.
The exact cause and mechanism of the pain in the absence of infection or inflammation are not fully understood. CPPS commonly affects men with an average age of 43, causing persistent discomfort in the perineum (the area between the scrotum and anus) and genitals. It is estimated that 2 to 16% of men experience CPPS, although men often tend to underreport or keep silent about genital-related issues.
CHRONIC PELVIC PAIN IN MEN SYMPTOMS
Pain is the most frequent complaint. Typically, individuals experience pelvic, perineal, or genital pain while urinating, having bowel movements, or engaging in sexual activity. The pain appears suddenly and must persist for at least three out of the last six months. It can be intense and is commonly felt in the perineal and genital area, although it may also be present in the lower abdomen, penis, scrotum, rectum, and lower back.
Occasionally, urination may become difficult, and pain during ejaculation is common. The main symptoms include perineal/pelvic pain, urinary difficulties, sexual problems like premature ejaculation and weaker erections, painful ejaculation, and systemic conditions such as muscle and joint pain, as well as unexplained fatigue. The symptoms of CPPS often vary irregularly, with periods of improvement followed by worsening.
CHRONIC PELVIC PAIN IN MEN DIAGNOSIS
A physical check-up can be performed to eliminate other disorders or conditions that might cause similar symptoms. The digital rectal examination (DRE) is the most crucial part of the check-up, assessing the prostate’s size, texture, symmetry, and sensitivity. Most CPPS patients will have normal DRE results. Laboratory tests can rule out any infection or inflammation. Imaging of the pelvis, like ultrasound, CT scan, and MRI, is often unnecessary but may help exclude conditions like abscesses, cysts, prostate cancer, and prostate stones.

CHRONIC PELVIC PAIN IN MEN – PHYSICAL THERAPY MANAGEMENT
Physical therapy provides a broad variety of techniques that are safe and effective for CPPS.
1 Pelvic Floor Muscle Training
The pelvic floor muscles create a dome-shaped structure that surrounds the pelvic cavity. This includes the area between your legs, extending from the front (penis) to the back (anus). These muscles serve multiple purposes such as stabilizing the pelvis, supporting internal organs, controlling bladder and bowel functions, and regulating erection, emission, and ejaculation. Similar to other muscles in the body, the pelvic floor muscles can experience spasms, trigger points, and resulting pain. Learning relaxation techniques to reduce muscle tension can help alleviate discomfort. In many cases, these muscles go into spasms due to weakness and lack of endurance. Working with a physical therapist to perform targeted exercises will help strengthen the pelvic floor muscles and reduce pain.
2. Acupuncture for Chronic Pelvic Pain in Men
Acupuncture can effectively alleviate pelvic pain in individuals diagnosed with CPPS by painlessly inserting needles at specific locations on the body.
3. Biofeedback
Learning to relax your pelvic floor and understanding when and how to contract these muscles can be beneficial for you. This painless method involves placing electrodes on the skin, which enables you to visually observe the muscle contractions on a computer screen. This visual feedback helps you learn the right sensation and timing for muscle contractions. Attending weekly or biweekly sessions of physical therapy for a total of six to eight treatments can lead to noticeable enhancements in muscle tone and a reduction in pain.
4. Myofascial Trigger Point Release for Chronic Pelvic Pain in Men
A skilled physiotherapist who specializes in pelvic floor treatment can carry out this procedure to alleviate muscle spasms and alleviate pain, ultimately enhancing muscle functionality. Research has demonstrated significant enhancements in symptoms subsequent to a trigger point release.
Chronic pain can have a significant impact, not only on your physical well-being but also on your mental and emotional state. It may cause feelings of anxiety and depression, affecting various aspects of your life such as work, social interactions, and physical activities. If CPPS is affecting your bowel or bladder control and your sexual health, it can be distressing, leading to feelings of shame, embarrassment, isolation, and strain on your personal relationships. Seeking support and discussing the emotional consequences of this pain and its physical symptoms can be highly beneficial. It is important to reach out for help and guidance, as there are effective measures to improve your symptoms. Remember that you are not alone in this journey.
Chronic Pelvic Pain in Men – PELVIC FLOOR EXERCISES
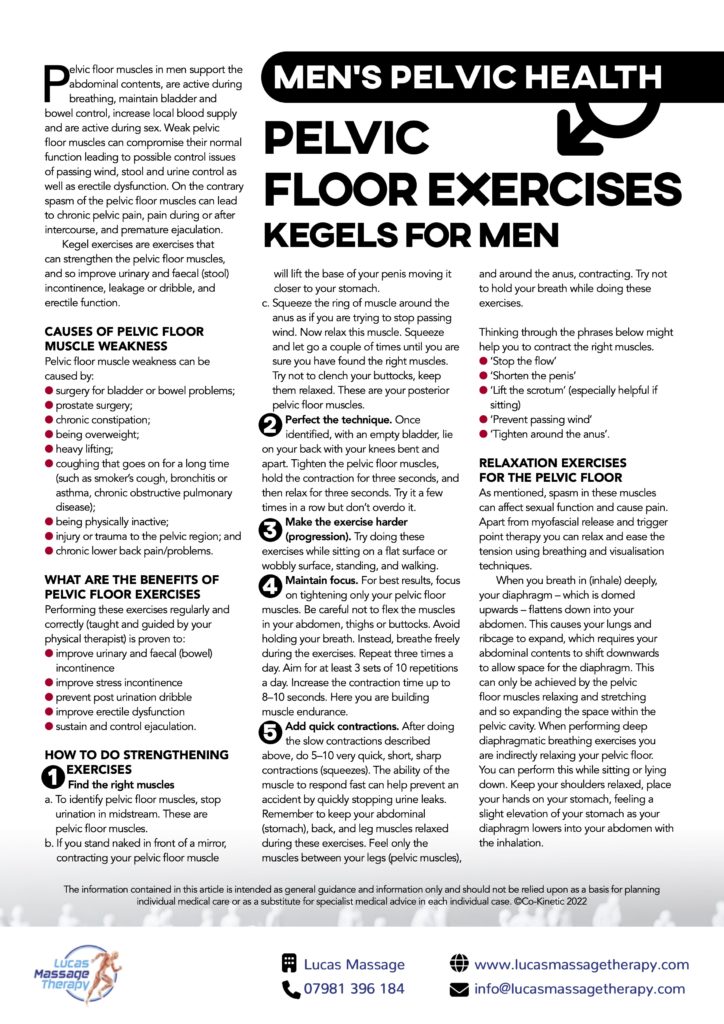
We’re talking bladder control, bowel movements and yep, the reproductive organs as well. All these crucial functions are controlled by muscles in the pelvis.
Dysfunction in any of these areas is something you need to see a doctor about asap. In some cases, symptoms can be a sign of a more serious health problem such as prostate cancer.
##What Are ‘Pelvic Health’ Problems?
Issues in the pelvic region vary greatly, from pain to leaky bladders or bowels to sexual dysfunction problems like premature ejaculation. They’re also more common than you might think, and most are easily managed or treated once medical help has been requested.
##FREE – Men’s Pelvic Health Resource Pack
Download our Lucas Massage Therapy free information pack and find out everything you need to know about men’s pelvic health.
What You’ll Learn:
- The different signs and symptoms to look out for in the pelvic region
- When symptoms might indicate prostate cancer
- How pelvic health conditions are treated
- The dangers of ‘staying silent’
- How a few simple exercises can make a big difference to your pelvic health

